Introduction
As we enter the cold and flu season in Canada, this article will outline why additional precautions for people with developmental disabilities have been so prevalent over the past 3 years as we have navigated not only COVID-19 but all Pulmonary Diseases.
If you have any questions, concerns or would like to add something to the discussion you can reach out to the Healthcare Strategies Manager at gcruncian@christian-horizons.org.
What is Pulmonary Disease?
Pulmonary Disease encompasses a variety of different infections or structural issues specific to the respiratory system. The respiratory system is not only the lungs but also includes the oral/naval cavity, trachea, right/left bronchus, right/left bronchioles and the alveolus. The diagram below from the Lung Association identifies all of the important landmarks.
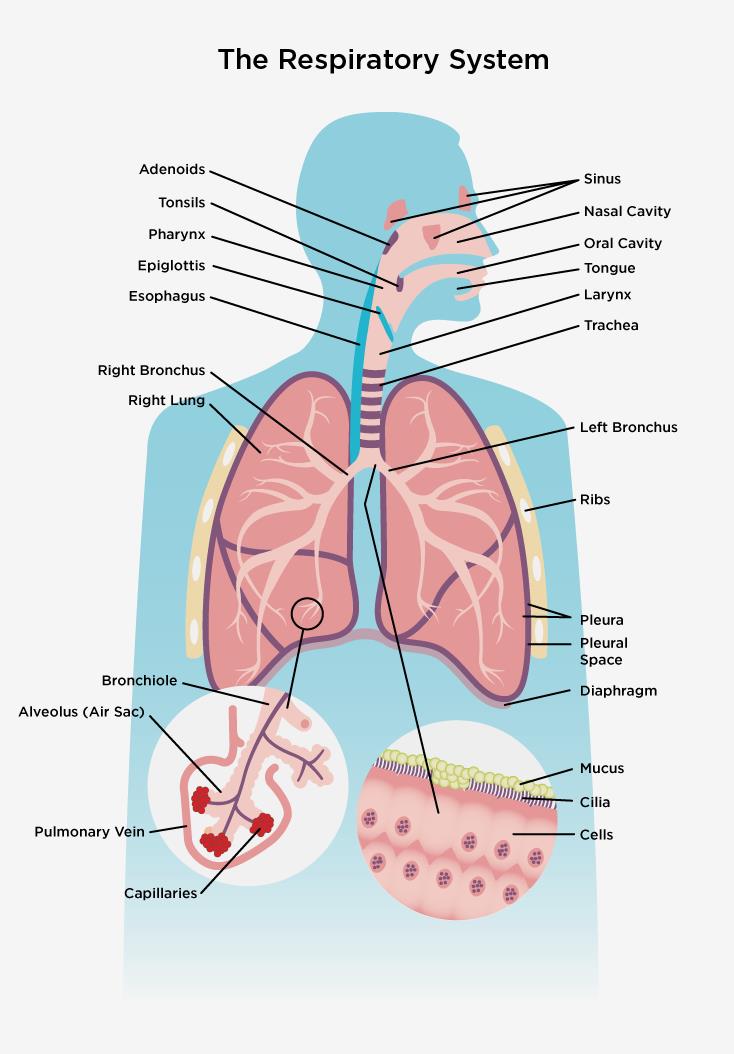
Source found here.
As we discuss pulmonary disease, a variety of resources will be utilized from different jurisdictions. While research on health outcomes for people with developmental disabilities continues to be a growing area in Canada, most of our guidelines are based on research done in other countries.
How Common is Pulmonary Disease in people with Developmental Disabilities?
People with developmental disabilities are at an increased risk for developing chronic pulmonary diseases throughout their lives. Chronic illnesses include asthma or chronic obstructive pulmonary disease (COPD). At the same time people with developmental disabilities are at an increased risk of negative health outcomes from acute pulmonary diseases such as colds, flu and COVID-19 (Source)
Due to the increased risk of not only chronic pulmonary disease but negative health outcomes, advocacy during medical appointments and more broadly with public health agencies continues to be an important component of supporting people with developmental disabilities.
Recognizing Pulmonary Disease
Pulmonary diseases affect the respiratory system. This results in changes to an individual’s ability to breath. Any of the following symptoms could be expected:
- Increasing Breathlessness
- Persistent “chesty” Cough with Phlegm.
- Wheezing (a high-pitched whistling sound made while breathing)
Prolonged and unimproved symptoms could be a sign of a chronic pulmonary disease.
Sudden onset of these symptoms could be the result of a cold, the flu or COVID-19. This is likely to be an issue during cough/cold season which typically lasts from October – April each year. To help differentiate between them, consider the below graphic.

Treatment
Treatment for pulmonary disease relies on determining what the underlying cause of the issue is and whether it is an acute or chronic issue. In the case of bacterial pneumonia, the treatment may require antibiotics. For Cold and Flu, treatment will typically focus on managing the symptoms and allowing the body’s own immune system to fight the infection. For COVID-19 there is the option of anti-viral medications specific to COVID-19 that can help lesson the severity of the illness.
More chronic illness, such as COPD, will focus on improving the overall quality of life for the person supported. This may include daily inhalers or supplemental oxygen. For those with asthma, the focus is often on avoiding triggers for asthma attacks and having “rescue inhalers” available in case of an asthma attack. Rescue inhalers are prescribed by a primary health care provider, to be used in situations when a person supported is having difficulty breathing.
Emergency Situations
Even with the best planning and unlimited supports, emergencies can occur with little or no warning.
When someone is in respiratory distress, the signs tend to be clear. The individual will be straining for breath, likely using accessory muscles to breath. When someone is using accessory muscles to breath it will appear as though they are breathing in an exaggerated way with their full chest expanding, shoulders lifting, and the abdomen expanding. The heart rate is likely to be increased and oxygen levels will decrease. People with a light complexion may show signs of cyanosis or “blue tinged skin” around the fingers and lips.
When emergencies occur the team should ensure the persons immediate safety and follow the care plan for next steps. The next steps may include:
- Administering any PRNs such as inhalers
- Calling emergency services (911).
Closing Thoughts
Pulmonary Disease is not only a seasonal issue, with many illnesses that affect an individual’s ability to breath, it is important that we are prepared to support them. With the increased risk of negative health outcomes for people with developmental disabilities, when they have pulmonary diseases it is necessary for teams to know how to identify pulmonary disease and how to support people when they are ill.
Breathe – The Lung Association. Respiratory System. (Source)
Surrey Place, Primary Care Guidelines, Respiratory Disorders (Source)